- Professional Development
- Medicine & Nursing
- Arts & Crafts
- Health & Wellbeing
- Personal Development
Good Clinical Practice (GCP) courses in Belfast
We couldn't find any listings for your search. Explore our online options below.
Know someone teaching this? Help them become an Educator on Cademy.
Online Options
Show all 53GXP01- Good Practices (GxP) in Drug Development and Manufacturing
By Zenosis
This short entry-level module introduces the learner to good practices (GxP) in drug development and manufacturing. It outlines how the industry operates and how it is regulated. It identifies regulatory authorities and other important sources of guidance on Good Manufacturing Practice (GMP), Good Clinical Practice (GCP), and Good Laboratory Practice (GLP).

GXP01: Good Practices (GxP) in Drug Development and Manufacturing
By Zenosis
This short entry-level module introduces the learner to good practices (GxP) in drug development and manufacturing. It outlines how the industry operates and how it is regulated. It identifies regulatory authorities and other important sources of guidance on Good Manufacturing Practice (GMP), Good Clinical Practice (GCP), and Good Laboratory Practice (GLP).

CT03a - ICH, harmonisation, and principles of Good Clinical Practice
By Zenosis
Good Clinical Practice (GCP) is a set of internationally recognised ethical and scientific quality requirements for designing, conducting, recording and reporting clinical trials. Compliance with GCP principles is required by regulatory authorities in many countries for the authorisation of clinical trials and the acceptance of their data in applications for marketing approval. The International Council for Harmonisation's guideline E6, often referred to as ICH GCP, is the international standard specification for Good Clinical Practice. In this short course we describe the ICH’s role in the harmonisation of regulations, introduce its guideline E6, and set out the principles of GCP.
CT03: ICH Good Clinical Practice
By Zenosis
Good Clinical Practice (GCP) is a set of internationally recognised ethical and scientific quality requirements for designing, conducting, recording and reporting clinical trials. Compliance with GCP principles is required by regulatory authorities in many countries for the authorisation of clinical trials and the acceptance of their data. The International Council for Harmonisation’s guideline E6, often referred to as ICH GCP, is the international standard specification for Good Clinical Practice.
CT09: Good Clinical Practice Inspections and Audits
By Zenosis
The module describes general principles of GCP inspection and audit, discusses preparation for an inspection, and sets out in detail what European and US FDA inspectors will examine. Finally it describes post-inspection actions by the regulator and the inspected party.

Good Clinical Practices: A Practical Guide to GCP Compliance
By Xpert Learning
About Course Understand the Ethical and Regulatory Framework for Conducting Clinical Trials Course Description This comprehensive Good Clinical Practices (GCP) course provides a thorough understanding of the ethical and regulatory principles governing clinical trials. It delves into the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) guidelines, ensuring you grasp the essential standards for conducting clinical research. Course Objectives By the end of this course, you will be able to: Articulate the definition, purpose, and historical context of GCP. Explain the importance of GCP in protecting human subjects and ensuring data integrity. Identify key international organizations involved in establishing GCP standards. Apply ethical principles and informed consent procedures in clinical research. Understand the ICH E6(R2) guidelines on Integrated Addendum to Good Clinical Practice. Design and conduct clinical trials according to ICH E8 and E9 guidelines. Manage and report clinical trial data in compliance with ICH E6(R2) guidelines. Implement safety monitoring and adverse event reporting procedures as per ICH E6(R2) and E6(R3) guidelines. Navigate regulatory compliance and inspections related to clinical trials. Target Audience This course is designed for individuals who: Are interested in pursuing a career in clinical research or clinical trial management. Work in the pharmaceutical, biotechnology, or medical device industry. Seek to gain a comprehensive understanding of GCP principles and practices. Prerequisites No prior experience in clinical research is required. However, a basic understanding of research methodology and medical terminology is recommended. Please Note: This course is strictly theoretical and does not qualify participants for clinical practice in the industry. Additional training and certifications may be required for hands-on experience. What Will You Learn? Articulate the definition, purpose, and historical context of GCP. Explain the importance of GCP in protecting human subjects and ensuring data integrity. Identify key international organizations involved in establishing GCP standards. Apply ethical principles and informed consent procedures in clinical research. Understand the ICH E6(R2) guidelines on Integrated Addendum to Good Clinical Practice. Design and conduct clinical trials according to ICH E8 and E9 guidelines. Manage and report clinical trial data in compliance with ICH E6(R2) guidelines. Implement safety monitoring and adverse event reporting procedures as per ICH E6(R2) and E6(R3) guidelines. Navigate regulatory compliance and inspections related to clinical trials. Course Content Introduction to Good Clinical Practice (GCP) and ICH Guidelines Introduction to Good Clinical Practice (GCP) and ICH Guidelines Ethical Principles, Informed Consent, and ICH E6(R2) Ethical Principles, Informed Consent, and ICH E6(R2) Designing and Conducting Clinical Trials with ICH E8 and E9 Designing and Conducting Clinical Trials with ICH E8 and E9 Data Management and Reporting with ICH E6(R2) Data Management and Reporting with ICH E6(R2) Safety and Monitoring in Clinical Trials with ICH E6(R2) and E6(R3) Safety and Monitoring in Clinical Trials with ICH E6(R2) and E6(R3) Regulatory Compliance, Inspections, and ICH E6(R3) Regulatory Compliance, Inspections, and ICH E6(R3) A course by Xpert Learning RequirementsA basic understanding of research methodology and medical terminology is recommended. Audience Individuals who are interested in pursuing a career in clinical research or clinical trial management. Individuals who work in the pharmaceutical, biotechnology, or medical device industry. Individuals who seek to gain a comprehensive understanding of GCP principles and practices. Audience Individuals who are interested in pursuing a career in clinical research or clinical trial management. Individuals who work in the pharmaceutical, biotechnology, or medical device industry. Individuals who seek to gain a comprehensive understanding of GCP principles and practices.

Good Clinical Practice Auditing - Principles and Practice
By Research Quality Association
Course Information Our comprehensive course is used as a gateway to those stepping into the world of auditing clinical studies. Tailored for those already acquainted with Good Clinical Practice (GCP) and those transitioning from other audit disciplines, this programme stands as a pivotal guide. Pre-existing knowledge of GCP will significantly enhance your learning experience in auditing against these guidelines. How is this course run? Engage in immersive workshops providing hands-on practice with auditing techniques in a GCP context. Our seasoned tutors, boasting extensive audit experience, intertwine theory with practical insights drawn from their own professional journeys. What will I learn? A comprehensive understanding of the historical backdrop and objectives driving Good Clinical Practice, incorporating the latest industry developments Solid grounding in quality assurance activities aligned with regulatory standards Insight into potential pitfalls within clinical trials and the pivotal role of auditors in addressing these issues Clarity on the roles and responsibilities inherent to clinical trials auditing Exposure to a diverse range of audit techniques complemented by illustrative examples and supportive documents A nuanced understanding of regulatory inspectors' activities Expanded professional networks to propel your auditing career forward. Benefits include: A clear understanding of the role of the auditor under Good Clinical Practice improved audits Improved Good Clinical Practice compliance for your clinical trials. This course is structured to encourage delegates to: Discuss and develop ideas Solve specific problems Examine particular aspects of Good Clinical Practice. Tutors Tutors will be comprised of (click the photos for biographies): Rosemarie Corrigan EVP Global Quality, Worldwide Clinical Trials Cathy Dove Director and Owner, Dove Quality Solutions Julie Kelly Associate Director, Clinical Quality Assurance, Corcept Therapeutics Susana Tavares Director of Research Quality Assurance, - Programme Please note timings may be subject to alteration. Day 1 12:30 Registration 13:00 Welcome and Objectives for the first day of the course 13:30 Laying the Foundations Introduction to the clinical development process, the concepts of quality assurance, quality control and audit. 14:30 Break 15:00 Patient Protection Requirements for informed consent and ethics committee. Access to source documentation. Including a patient protection exercise. 16:05 Workshop 1 - Case Study on Informed Consent 16:45 End of Day Questions and Answers 17:00 Close of Day Day 2 08:50 Questions and Answers from Day 1 09:00 Effective Site Audits The procedures involved in selecting and setting up audits at investigator sites. 09:40 Workshop 1 - Planning the Effective Audit 10:30 Break 10:45 Source Data Verification The need for and purpose of verifying data. 11:25 Workshop 2 - Source Data Verification 12:30 Lunch 13:30 IMP Management The requirements surrounding the distribution of investigational medicinal products. Accountability from release to destruction. 14:15 Critical Document Audits The conduct of other study specific audits including protocols, databases and reports. 15:00 Break 15:15 Non-compliance Determining the acceptability of data. 16:00 Fraud - Fact or Fiction? How to identify fraud and its consequences 16:45 End of Day Questions and Answers 17:00 Close of Day Day 3 08:50 Questions and Answers from Days 1 and 2 09:00 Auditing Third Parties A review of audits of contract research organisations. 10:00 System Audits The concept of auditing processes across many clinical trials, including a practical exercise in process mapping. 10:45 Break 11:00 Workshop 3 - Process Mapping 11:45 Effective Audits Where theory meets reality. 12:30 Lunch 13:20 Audit Reports - Closing the Loop An examination of the processes which follow the evidence gathering phase of the audit. 14:20 Workshop 4 - Audit Reports Audit reports, corrective and preventive action. 15:00 Break 15:10 Regulatory Inspection Auditors and regulatory inspections -how the QA team can help the organisation to perform during a regulatory inspection. 15:55 Final Questions and Answers 16:10 Close of Course Extra Information Face-to-face course Course Material Course material will be available in PDF format for delegates attending this course. The advantages of this include: Ability for delegates to keep material on a mobile device Ability to review material at any time pre and post course Environmental benefits – less paper being used per course. The material will be emailed in advance of the course and RQA will not be providing any printed copies of the course notes during the training itself. Delegates wishing to have a hard copy of the notes should print these in advance to bring with them. Alternatively delegates are welcome to bring along their own portable devices to view the material during the training sessions. Remote course Course Material This course will be run completely online. You will receive an email with a link to our online system, which will house your licensed course materials and access to the remote event. Please note this course will run in UK timezone. The advantages of this include: Ability for delegates to keep material on a mobile device Ability to review material at any time pre and post course Environmental benefits – less paper being used per course Access to an online course group to enhance networking. You will need a stable internet connection, a microphone and a webcam. CPD Points 17 Points Development Level Develop

GCP Good Clinical Practice
By NBScience
GCP Good Clinical Practice

The Remote Auditing Course
By Research Quality Association
Course Information Join us for a two-day immersive course crafted to equip participants with an in-depth understanding of remote audit methodologies. Delve into the nuances between remote and face-to-face audits, dissecting their respective strengths and limitations. Through practical scenarios tailored for remote audit conduct, this course stands as an essential counterpart to our on-site audits course The Auditing Course. Who Should Attend: Applicable across various domains of regulated research and development, this course proves invaluable in contexts requiring a quality system for audit. Participants with firsthand audit experience stand to gain the most benefit from this programme. Expanding on Previous Learning: This course extends its relevance to all forms of audits and further amplifies concepts explored in RQA's suite of research quality assurance courses, including: 'Research Quality Assurance for Good Laboratory Practice,' 'Good Clinical Practice Auditing – Principles and Practice,' and 'Good Manufacturing Practice for Investigational Medicinal Products.' Benefits include improved: Understand the processes of planning, conducting, reporting and follow-up of audits Recognising the importance of personal approach in developing positive audit outcomes Ability to analyse evidence and present logical audit findings Appreciate the importance of audit in continuing improvement. This course is structured to encourage delegates to: Discuss and develop ideas Solve problems Exchange information. Tutors Tutors will be comprised of (click the photos for biographies): Andrew Waddell Founder Director, Tower Mains Ltd Rosemary Ichaba Senior QA Associate, Tower Mains Ltd Cate Ovington Director, The Knowlogy Group Ltd Jean McWilliam Associate Director, Alexion Programme Please note timings may be subject to alteration. Day 1 09:00 Course Registration 09:15 Welcome and Introductions 09:35 Introduction to Audits Delegates explore the range of audits which they have experienced, define the purpose of each audit type and establish which of those audits are performed to meet regulatory requirements. 10:05 Introduction to Remote Audits Presentation to introduce the major differences between face-to-face audits and remote audits. The major elements of audits will be examined to determine where there may be differences. 10:30 Break 10:45 Workshop 1 - Remote Audits This workshop will examine participants experience or understanding of the differences between face-to-face and remote audits. 11:15 Workshop 1 - Feedback 11:35 Audit Preparation The essential steps in preparation for audits will be discussed with emphasis on remote audits. 12:05 Workshop 2 - Remote Audit Preparation Factors relating to the preparation for remote audits will be considered in discussion groups. 12:35 Workshop 2 - Feedback 12:50 Lunch 13:30 Audit Logistics Preparation for the audit includes many arrangements other than the audit content. 14:00 Workshop 3 - Audit Logistics Delegates will discuss some of the issues that may occur during the set up and conduct of remote audits and how to resolve them. 14:30 Workshop 3 - Feedback 14:45 Break 15:00 The Opening Meeting Presentation regarding the importance and content of the opening meeting. 15:20 Workshop 4 - Opening Meeting Delegates will consider the practicalities of arranging and conducting an opening meeting. 15:45 Workshop 4 - Feedback 16:10 Audit Conduct Tools Practical advice on preparation of some of the tools that will be valuable in the conduct of audits. 16:40 Questions and Answers An overview of the first day and a chance to ask questions 17:00 Close of Day Day 2 09:00 Reflections on Day 1 Recap on the topics covered and a chance for delegates to raise points. 09:15 Gathering Evidence Presentation on challenges of gathering evidence and conducting interviews during remote audits. 09:45 Workshop 5 - Remote Interviews Scenarios of different remote interviews will be played and delegates assess the strengths and weaknesses of each approach. 10:15 Break 10:30 Creating Audit Findings Ideas regarding how to create good audit findings will be discussed during this short presentation. 10:50 Workshop 6 - Creating Audit Findings Delegates will be provided with examples of evidence from an audit. They will discuss these and create their audit findings for presentation at the closing meeting. 11:35 The Closing Meeting The content and conduct of the closing meeting will be discussed. 11:55 Workshop 7(a) - Preparing for the Closing Meeting The findings from workshop 6 will be reviewed and a Lead Auditor selected to provide feedback in workshop 7(b) 12:15 Workshop 7(b) - The Closing Meeting The Lead Auditor from each group will hold a meeting to present the results (role play). 12:45 Lunch 13:30 The Audit Report This presentation will cover not only the essential contents of the audit report but also how to write the report in a manner that will generate the most positive reaction. 14:00 Workshop 8 - The Audit Report Delegates will be provided with an audit report from an audit conducted remotely and will conduct a peer review of the report in their breakout groups. 15:00 Workshop 8 - Feedback 15:20 Break 15:35 Audit Closure Presentation on how to conclude the audit with reference to post-audit activities. 15:55 Open Forum 16:30 Close of Course Extra Information Course material This course will be run completely online. You will receive an email with a link to our online system, which will house your licensed course materials and access to the remote event. Please note this course will run in UK timezone. The advantages of this include: Ability for delegates to keep material on a mobile device Ability to review material at any time pre and post course Environmental benefits – less paper being used per course Access to an online course group to enhance networking You will need a stable internet connection, a microphone and a webcam.

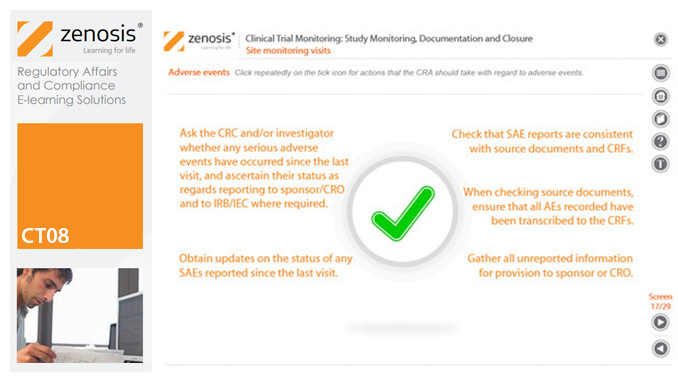
CT08: Clinical Trial Monitoring: Study Monitoring, Documentation and Closure
By Zenosis
The sponsor of a clinical trial must arrange for it to be monitored throughout its duration to ensure that the rights and wellbeing of subjects are protected, the trial data are accurate, complete and verified from source documents, and the conduct of the trial complies with the study protocol, Good Clinical Practice and regulatory requirements. In this module we describe how a Clinical Research Associate (CRA) monitors an ongoing trial to its conclusion.
Search By Location
- Good Clinical Practice (GCP) Courses in London
- Good Clinical Practice (GCP) Courses in Birmingham
- Good Clinical Practice (GCP) Courses in Glasgow
- Good Clinical Practice (GCP) Courses in Liverpool
- Good Clinical Practice (GCP) Courses in Bristol
- Good Clinical Practice (GCP) Courses in Manchester
- Good Clinical Practice (GCP) Courses in Sheffield
- Good Clinical Practice (GCP) Courses in Leeds
- Good Clinical Practice (GCP) Courses in Edinburgh
- Good Clinical Practice (GCP) Courses in Leicester
- Good Clinical Practice (GCP) Courses in Coventry
- Good Clinical Practice (GCP) Courses in Bradford
- Good Clinical Practice (GCP) Courses in Cardiff
- Good Clinical Practice (GCP) Courses in Belfast
- Good Clinical Practice (GCP) Courses in Nottingham